Empowering Dual Eligible Consumers through Information Exchange:
Early Lessons from Cal MediConnect
By Janet Heinritz-Canterbury, M. S.W., Greg Thompson, M.S.W. March 2015
PASCBackground
The Personal Assistance Services Council is the Los Angeles County In-Home Supportive Services (IHSS) public authority. Over 190,000 LA County seniors and people with disabilities receive IHSS services from over 130,000 providers. IHSS is a Medi-Cal benefit started in the 1970s and the cornerstone of IHSS is the
consumer-directed foundation of the program; consumers are experts on their own lives; they are the ones who are best able to direct the services they receive. IHSS has helped make it possible for people with disabilities and seniors to live productive lives in the community without being forced into institutions. Through PASC’s provider registry, monthly telephone town halls, and on-going consumer outreach and training programs, PASC connects with thousands of IHSS recipients and hears their concerns, complaints, fears, and suggestions about IHSS. Over the past several years, IHSS consumers have experienced massive changes including cuts in their IHSS service hours, a new payroll process for their IHSS providers, and, a newly structured health care program
with the launching of Cal MediConnect 1 in April 2014. Cal MediConnect is for people who are on both Medicare and Medi-Cal, and it coordinates services from both of these programs. In this workshop, we look at the communication strategies PASC utilized with these IHSS recipients concerning Cal MediConnect and some of the lessons that we learned from those communications.
Cal MediConnect
Cal MediConnect is a new kind of managed care plan that combines Medicare and Medi-Cal services for people who receive services from both programs. This population is primarily seniors and people with disabilities who are particularly vulnerable, at-risk, and highly medicated. Eligible individuals can opt out of Cal MediConnect for their Medicare services-that is, they can keep their doctors and specialists and services paid for by Medicare-but they must select a Medi-Cal Only plan for services provided by Medi-Cal, including their long term services and supports. Ifthe eligible individual does not make a decision and convey that decision to the State, the State will make a choice for the individual-they will enroll the person into a Cal MediConnect plan. Conveying the facts and choices of this program can be problematic because of people’s fear of something new, suspicion of government making a choice for them, overall distrust of and misinformation about managed care, read more..
[hr]
Los Angeles CCI Communications Work Group
IHSS Phone Bank at PASC Offices in Pasadena
Wednesday, November 12, 2014
Brief Summary
After months of planning and coordination, the LA CCI Communications Work Group implemented a phone bank for IHSS recipients with questions on their CCI enrollment decision. In the months leading up to the November 12th phone bank, the Work Group, made up of over a dozen Advocacy Groups, Agencies, and the LA County Cal MediConnect plans, wrangled over how to get information to IHSS recipients. With input and funding from all stakeholders, the phone bank plan included a letter from PASC mailed in early November to over 16,000 IHSS recipients with December birthdays giving them a two hour time period on Wednesday evening, November 12th to call PASC and talk with an informed and unbiased person about their CCI decision.
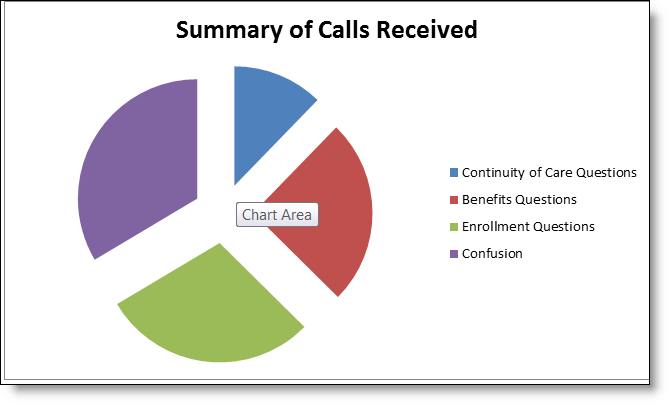
Using PASC’s Registry Call Center in Pasadena, 24 volunteer phone bankers took calls from over 200 IHSS consumers, family members, and IHSS providers from 6:00 pm until 8:00 pm and PASC took calls from another 100 consumers on days before and after the phone bank. The goal of the calls was to move the caller to action in finding the information they needed for their decision. The phone bankers listened to the consumer’s question and then helped the caller decide how to get the information to answer their question about enrollment, benefits, continuity of care, or other issues. While the volunteer phone bankers were all familiar with the CCI and Cal MediConnect, they were careful not to market about any specific plan or suggest any specific choice for the caller. In a brief training, phone bankers were instructed avoid the “weeds” and political wrangling with the callers—instead try to move them to action on their question. Phone bankers asked callers if they wanted information mailed to them and if they knew what they would do the next day on their question.
PASC IT staff provided 24 phones with 6 of the 24 designated for both Spanish and English callers. The callers heard a message allowing them to choose a language and then routed them to an available phone banker. If all lines were busy the caller was placed into a queue with an option to hold or leave a message. Each phone banker had a phone and a computer with an excel spreadsheet for phone bankers to record data from each call. The spreadsheet included caller’s contact information; caller’s question—continuity of care, benefits, confusion, and other; did they want information mailed to them; did they know what to do to get the information they needed; and was this call helpful. A caller could have concerns in any or all of these areas.